MN-166 for ALS
Last updated Nov. 27, 2024, by Marisa Wexler, MS

What is MN-166 for ALS?
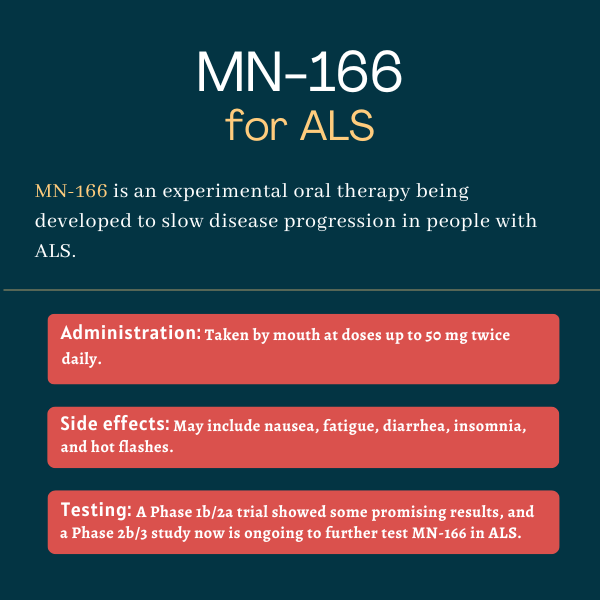
MN-166 (ibudilast) is an oral anti-inflammatory molecule that’s designed to reduce inflammation and protect nerve cells from damage in people with amyotrophic lateral sclerosis (ALS). This is expected to slow disease progression.
MN-166, which is being tested in ALS in a Phase 2b/3 clinical trial, has been granted fast track designation by the U.S. Food and Drug Administration for this indication. Such designation aims to speed the development and review of new therapies that may treat serious conditions with an unmeet medical need.
MN-166 also has received orphan drug designation in both the U.S. and Europe, a status that provides incentives for companies developing treatments for rare disorders, including several years of market exclusivity if the therapy is ultimately approved.
MediciNova is developing MN-166 for ALS as well as progressive multiple sclerosis and substance abuse. The molecule originally was developed by Kyorin Pharmaceutical, and it has been approved in Japan since 1989 to help with complications after stroke and with certain types of asthma.
Therapy snapshot
| Treatment name: | MN-166 |
| Administration: | Oral tablets |
| Clinical testing: | Being tested in an ongoing Phase 2b/3 trial |
How does MN-166 work in ALS?
In ALS, motor neurons, the specialized nerve cells responsible for controlling voluntary movements, become damaged and die, resulting in muscle weakness and other disease symptoms.
The exact causes of ALS aren’t fully understood, but abnormal inflammation is thought to play a central role in the death and degeneration of motor neurons in patients.
The active agent in MN-166, ibudilast, is designed to reduce immune cell activity in the brain and boost the survival and growth of nerve cells. It does that by targeting four proteins — phosphodiesterase-3, -4, and -10, as well as macrophage migration inhibitory factor — that are released by white blood cells into the bloodstream to set off an immune response. It also blocks the activity of toll-like receptor 4, which is a sensor protein that drives inflammation.
Studies in animal models have shown that MN-166 can enter the brain and spinal cord, where it reduces the activation of glial cells, supportive nerve cells that become abnormally active in neurodegenerative conditions, and exerts neuroprotective effects.
Through these mechanisms, it’s hoped that MN-166 can help to lessen the damage to motor neurons that drives ALS, ultimately slowing disease progression.
How will MN-166 be administered in ALS?
MN-166 is an oral medication that has been given as oral tablets, each containing 10 mg of the active therapy. It now is being tested as oral capsules containing the same amount of the medication.
The treatment has been tested in a Phase 1b/2a trial at daily doses of up to 60 mg. But participants in the ongoing Phase 2b/3 study are receiving a 50 mg dose twice daily (or 100 mg daily).
MediciNova also is developing a novel formulation of MN-166 that’s given via an intravenous, or into-the-vein, infusion for those with ALS or other conditions who cannot swallow the oral capsules. That formulation has been found to be safe and well tolerated in healthy volunteers, but it has not yet been tested in people with ALS.
It’s unclear if the company will seek the approval of both formulations, and it’s also too soon to know which dose and regimen will be used in the clinic if MN-166 ultimately is approved for ALS.
MN-166 in ALS clinical trials
MediciNova has tested MN-166 as an add-on to standard ALS treatments in a Phase 1b/2a clinical trial and an exploratory Phase 1b biomarker study. A Phase 2b/3 trial is ongoing.
Phase 1b/2a study
A Phase 1b/2a clinical trial, called IBU-ALS-1201 (NCT02238626), tested MN-166 as an add-on to the approved ALS treatment Rilutek, the tablet formulation of riluzole.
The study enrolled 51 patients at a single center in the U.S., who were randomly assigned to take MN-166 at a dose of 60 mg/day (30 mg twice daily), or a placebo, for six months. This was followed by a six-month open-label extension period where all were given MN-166 plus Rilutek.
The trial’s main goal was to evaluate the safety of MN-166 plus Rilutek, and results were positive, with no serious side effects related to MN-166.
Trial investigators also explored the treatment’s effect on disease progression, as measured with the ALS Functional Rating Scale-Revised (ALSFRS-R), as well as changes in muscle strength and quality of life. Results showed no overall differences in any of these measures between patients on MN-166 or a placebo.
However, post hoc analyses, which are those designed and carried out after a trial is over and all data are available, suggested that more patients given MN-166 than a placebo had stable or improved scores on the ALSFRS-R scale (21.2% vs. 12.5%). The proportion of patients with stable or improved quality of life scores also was greater with MN-166 (51.5% vs. 25%).
Long-term data from the study suggested that MN-166 tended to extend survival compared with Rilutek alone, suggesting a possible survival benefit.
Phase 1b biomarker study
The exploratory Phase 1b biomarker study (NCT02714036) tested MN-166, at a dose of 30-50 mg twice daily, in 35 people with ALS for about eight months. All could continue to receive riluzole during that period.
The study investigated the treatment’s effect on markers of nerve damage and immune cell activation in the brain, but results found no significant effect on these biomarkers. Still, it showed that daily doses of up to 100 mg had an acceptable safety and tolerability profile.
Phase 2b/3 COMBAT-ALS trial
An ongoing Phase 2b/3 trial called COMBAT-ALS (NCT04057898) is further exploring the safety and efficacy of MN-166 in about 230 ALS patients, ages 18-80, who experienced their first ALS symptoms no more than 18 months before entering the study.
Participants are being randomly assigned to take MN-166 — at a dose of 30 mg twice daily for two weeks and up to 50 mg twice daily thereafter — or a placebo for one year. All then may choose to take MN-166 for an additional six months.
Throughout the study, patients on a stable dose of riluzole and/or edaravone (sold as Radicava and Radicava ORS) may continue receiving those medications.
Its main goal is to compare changes in ALSFRS-R scores after one year. Secondary assessments include changes in muscle strength and quality of life, the proportion of patients with stable or improved ALSFRS-R scores, and time to death or needing permanent ventilatory support. Safety will also be examined.
Common side effects of MN-166
In early ALS clinical trials, the most common side effects that were deemed possibly related to MN-166 included:
- nausea
- fatigue
- diarrhea
- insomnia
- hot flashes.
Some patients also experienced serious adverse events, but these were all common to ALS progression and not considered related to treatment.
ALS News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Prioritizing comfort as we continue settling in for the ride with ALS
- Clene working with FDA on accelerated approval for CNM-Au8
- An author discusses ALS and how she became an activist
- Longitude Prize on ALS encourages use of AI to find new treatments
- Living near toxic algal blooms tied to shorter survival in ALS patients
Related articles






