NurOwn of ‘Meaningful’ Benefit to Earlier Stage Patients, Data Show

Brainstorm Cell Therapeutics‘ investigational cell-based therapy, NurOwn, might be able to slow disease progression and be of “meaningful” benefit to people with less severe amyotrophic lateral sclerosis (ALS), according to new analyses of Phase 3 trial data.
The company announced last year that its Phase 3 trial (NCT03280056) had failed to meet its primary goal of slowing disease progression in treated patients relative to those given a placebo. The U.S. Food and Drug Administration, after its initial review, agreed that data did not support NurOwn’s approval.
Trial researchers now used different methods to identify patients with less severe disease, and their analyses found a greater proportion of responders among early-stage ALS patients given NurOwn and a “potential for a meaningful treatment effect,” BrainStorm stated in a press release.
“This is an important finding, especially since this effect was protected by randomization,” said Stacy Lindborg, PhD, the company’s executive vice president and chief development officer. Being protected by randomization means that the results were not affected by potential confounding factors or bias.
“These compelling analyses add to the positive momentum behind our ALS program, and we were pleased to have the opportunity to share them with the clinical community,” Lindborg added.
Jonathan Katz, MD, a co-principal trial investigator and the director of the Forbes Norris ALS Clinic at California Pacific Medical Center, presented the results at the 4th Annual ALS One research Symposium, held virtually on Nov. 29–30.
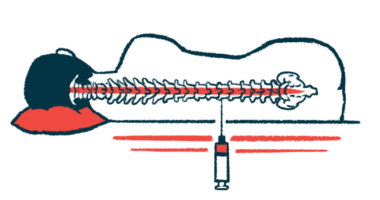
NurOwn is a cell therapy that uses mesenchymal stem cells (MSCs) isolated from a patient’s bone marrow. These cells are capable of maturing into many other cell types, and produce a variety of anti-inflammatory signaling molecules.
MSCs taken from the bone marrow are grown in the lab and matured into cells that produce large amounts of neurotrophic factors — compounds that promote nervous tissue growth and survival. The modified cells are then injected in the patient’s spinal canal.
The recently completed Phase 3 trial evaluated the safety and effectiveness of NurOwn in 189 people with rapidly progressing ALS. Participants were randomly assigned to a total of three injections of either NurOwn or a placebo, given directly into the spinal canal every other month.
Before starting treatment, patients were evaluated over 12 weeks to determine their rate of decline using the ALS Functional Rating Scale (ALSFRS-R) score.
ALSFRS-R, a measure of disease progression, assesses such daily life abilities as swallowing, speaking, dressing and washing oneself, climbing stairs, and turning over in bed. Each function is scored from 0 to 4, with a maximum total score of 48. Higher scores indicate better functional abilities.
The trial’s main efficacy goal was to determine NurOwn’s superiority to placebo through the proportion of patients with at least a 1.25-point slower rate of decline in ALSFRS-R at 28 weeks — about seven months — after a first dose.
Secondary goals included the proportion of patients whose disease had not progressed, total ALSFRS-R decline, and a combined analysis of function and survival. Other secondary goals were tracheostomy-free and overall survival, and the levels of biomarkers in the cerebrospinal fluid (CSF; the liquid that surrounds the brain and spinal cord).
Top-line results, announced in November 2020, showed slower disease progression in a greater proportion of NurOwn-treated patients (34.7%) than those given a placebo (27.7%). However, these findings failed to reach statistical significance, meaning that this difference was most likely due to chance. Other secondary endpoints also were not met.
According to BrainStorm, the Phase 3 trial included a greater percentage of people at the study’s start with advanced ALS (ALSFRS-R scores of 25 or lower) than had other ALS studies.
Its data also demonstrated that patients with less advanced disease at the study’s start — meaning a baseline ALSFRS-R of 35 or greater — appeared to benefit from NurOwn. In this specific patient group, 34.6% of those given NurOwn had a slower disease progression compared with 15.6% of those on a placebo.
The researchers now validated these findings by examining a subgroup of patients predicted to have long or very long survival on the ENCALS prediction model. In this group, more patients were responding to NurOwn (33%) than to a placebo (14%).
Further analyses taking into account both the ALSFRS-R and ENCALS model categories suggest that the trial’s efficacy measures are impacted by severe disease.
“We are very encouraged by the observation that there appears to be a meaningful treatment effect in patients with less severe disease at baseline that is consistent when using baseline ALSFRS-R scores and the ENCALS model which incorporates additional important disease characteristics that have been shown to be predictive of survival time,” Lindborg said.
“Looking ahead, we are eager to share additional analyses from our Phase 3 trial with the clinical community through a peer reviewed publication and remain committed to pursuing the best and most expeditious path forward to bring NurOwn to patients with ALS,” she added.