Blocking Astrocyte Protein May Slow ALS Progression, Study Finds
Blocking channels containing the connexin 43 (Cx43) protein on astrocytes — a type of nerve support cell — slowed disease progression in a mouse model of amyotrophic lateral sclerosis (ALS), a study found.
The protein was found to be increased in ALS patient tissues and spinal fluid, and its presence on astrocytes could directly contribute to nerve cell death in cell cultures, according to the study.
“This is a new pathway that we have shown to be present in ALS tissues, animal models and patient-derived stem cells,” Nicholas Maragakis, MD, a professor at Johns Hopkins University and the study’s senior investigator, said in a university press release.
“It’s also exciting that this particular [channel] protein seems to be elevated in spinal fluid from patients with ALS and could serve as an important biomarker. This is a true precision medicine approach toward the disease,” Maragakis said.
The study, “Cx43 hemichannels contribute to astrocyte-mediated toxicity in sporadic and familial ALS,” was published in PNAS.
It’s been hypothesized that star-shaped nervous system cells called astrocytes can contribute to the death of motor neurons, cells responsible for voluntary movement, which are damaged and lost in ALS.
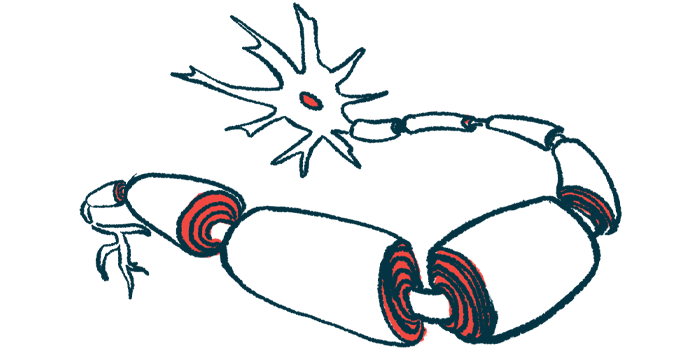
One of the ways astrocytes communicate with neighboring cells is through pore-like hemichannels that enable them to send signaling molecules directly into other cells.
Cx43 is a key component of these channels that’s been found to be elevated in the spinal cord of a mouse model of ALS. Blocking this molecule in astrocytes carrying ALS-related mutations seems to protect nerve cells from damage.
The research team led by scientists at Johns Hopkins University looked at whether Cx43 can contribute to ALS and if it could be a potential target for disease treatments.
Their study was funded by the ALS Association, the U.S. Department of Defense and the National Institutes of Health, the Maryland Stem Cell Research Fund, and the Robert Packard Center for ALS Research at Johns Hopkins.
The team demonstrated that depleting Cx43 from astrocytes significantly extended the survival of an ALS mouse model carrying a SOD1 mutation. The depletion didn’t delay the onset of disease in these animals, but it did prevent the loss of hind limb strength in the disease’s later stages and preserved motor neurons in the spinal cord’s cervical region.
The researchers also examined cerebrospinal fluid (CSF) — the fluid surrounding the brain and spinal cord — as well as brain and spinal cord samples from ALS patients. Cx43 was elevated in tissue and CSF from these patients, with the highest levels observed in those whose disease was progressing more rapidly.
The team also obtained stem cells from patients with sporadic or familial ALS and used them to generate astrocytes in cell cultures. Cx43 levels were increased in patient-derived astrocytes compared with healthy astrocytes, and higher levels were associated with more severe disease-causing mutations among those with familial forms of the disease.
Importantly, the astrocytes derived from ALS patients caused significant neuronal death when placed in culture with motor neurons. The neurodegenerative properties appeared to be mediated by Cx43-containing channels, which were highly present on the surface of astrocytes, and appeared more open, enabling more potentially toxic molecules to be transported to neighboring cells.
Together, the findings pointed to Cx43-containing channels as a promising target for ALS therapeutics, the researchers suggested.
Their theory was tested by adding tonabersat, a known blocker of Cx43-containing channels that’s been tested in the clinic, to the cultures containing motor neurons and patient-derived astrocytes.
Tonabersat significantly protected motor neurons and other nerve cells from degeneration. Plus, electrical recordings of the neurons showed their rate of firing was markedly reduced with tonabersat. Excessive firing, or hyperexcitability, of neurons is a known disease feature in ALS.
In the ALS animal models with SOD1 mutations, daily tonabersat treatment before symptom onset reduced levels of reactive gliosis, a process wherein astrocytes and microglia, another type of nerve support cell, are activated and cause inflammation.
The treatment also preserved motor neurons in the cervical spinal cord in later disease stages, suggesting that it slows disease progression, the researchers said. Reduced forelimb grip strength, indicative of muscle decline and disease progression in the model, appeared to be improved with tonabersat, although it was not statistically significant.
Similar results were observed when the treatment was given after the emergence of ALS symptoms. Chronic administration of tonabersat did not appear to be toxic.
The results demonstrate “the importance of Cx43 HC [channels] as contributors to ALS astrocyte-mediated neurotoxicity,” the researchers wrote. “The findings of this study offer potential for using Cx43 HC blockade for mediating ALS progression.”
The research team will next study why these channels are so active in ALS, with the hope that their findings will provide a better understanding of ALS progression, Maragakis said.