Nervous System’s Cardiac Control Response Depends on Type of ALS, Study Shows
Written by |
A nervous system mechanism that helps control heart rate and blood pressure goes into overdrive in patients with a type of ALS that eliminates mobility and sensation in some limbs, a study reports.
The control mechanism is known as sympathetic vascular response — with vascular response referring to heart blood vessels. The type of ALS is called flail arm or flail leg syndrome, depending on the limb involved.
Researchers’ key finding was that sympathetic vascular response increases in patients with a flail limb syndrome. The main indication of that was jumps in patients’ blood pressure during an experiment dealing with heart and blood pressure activity.
Researchers published their article in the journal Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration. The title is “Sympathetic vascular response to facial cooling is increased in flail phenotypes of amyotrophic lateral sclerosis.”
The different types of ALS include the classic version and rare versions such as flail arm or flail leg syndrome. A fail limb is one whose primary nerve has been severed, leaving no mobility or sensation.
Because flail limb syndrome is rare, scientists know less about its symptoms and the outlook for those who have it than they do about those with more common forms of amyotrophic lateral sclerosis.
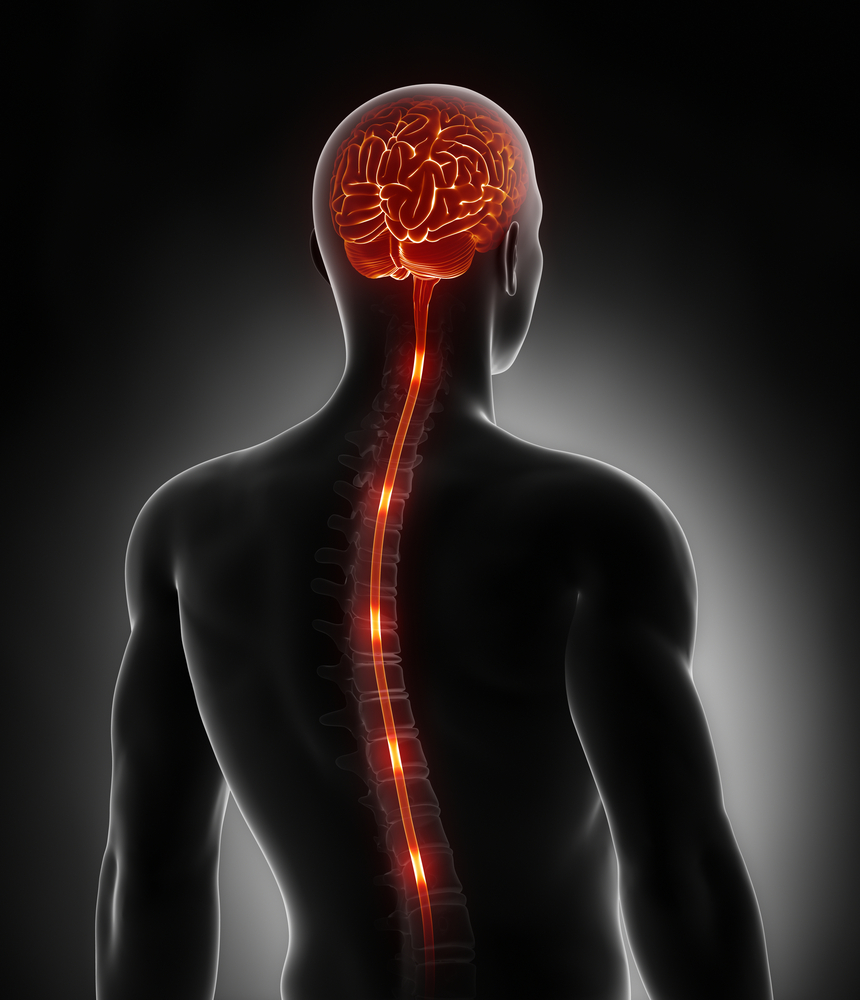
ALS is a multi-system neurodegenerative disorder. Part of the nervous system that it affects governs cardiac function, including heart rate and blood pressure. What scientists call the cardiovascular autonomic nervous system, or ANS, controls the nerves that regulate blood vessels in addition to the heart.
Studies have shown that the cardiovascular autonomic nervous system is unable to function properly in patients with classic ALS. A research team wanted to know how ANS functions in patients with flail limb versions of the disease.
ALS prevents people from taking standard cardiac function tests, however. Such tests require standing, taking deep breaths and doing other tasks that ALS disability rules out.
So researchers used what’s called the cold face test to determine the cardiac function of patients with flail limb syndrome. It involves cooling the forehead to activate pathways that slow the heart rate and increase blood pressure.
The study involved 18 people with classic ALS, eight with a flail limb form of the disease, and 10 age-matched controls. Researchers measured patients’ heart rate and took three types of blood pressure readings during two minutes of activity and one minute of a cold stimulus being applied to patients’ foreheads. The blood pressure measurements were systolic, diastolic, and mean blood pressure.
Researchers discovered no differences in the heart rate and blood pressure readings in classic and flail limb patients and in the controls before the experiment began.
All participants showed heart rate decreases and blood pressure increases when a cold stimulus was applied to their foreheads. The blood pressure increases were much larger in the flail limb ALS group than in the controls.
Another finding was that the time it took for blood pressure to increase in response to the cold stimulus was much shorter in flail limb patients than in classic ALS patients. The increase also lasted longer in the flail limb group than in the classic group.
Since blood pressure is associated with sympathetic vascular response, the results indicated that the hyperactivity that researchers saw in the heart rate and blood pressure control system occurred only in those with a flail limb type of ALS.
“Our results support the concept of ALS as a diffuse disease,” the team wrote. The study demonstrated that blood pressure hyperactivity was most pronounced in the flail limb versions of ALS, they added.