Study uncovers 2 therapies to help target autoimmune inflammation
UCLA researchers propose DMF, experimental H-151 for clinical testing
Dimethyl fumarate (DMF) — an oral medication approved for multiple sclerosis — and H-151, an experimental treatment, can suppress inflammatory and abnormal immune pathways thought to be involved in sporadic amyotrophic lateral sclerosis (ALS).
These are the findings of a study using immune cells from sporadic ALS patients that also showed DMF worked better when given in combination with epoxyeicosatrienoic acids (EETs), signaling fatty molecules that can be found in certain foods.
The results suggest DMF, in combination with a diet rich in certain fatty molecules, and H-151 could be therapeutic candidates for sporadic ALS patients not responding to currently available therapies, according to a research team led by scientists at the University of California, Los Angeles (UCLA).
Researchers plan to file application to test medications in clinical trial
With these preclinical data, the researchers plan to file an application to test the medications in a clinical trial, according to a UCLA press release. But before moving to clinical testing, they’ll do more research on immune cells of more patients.
The study, “Therapy of autoimmune inflammation in sporadic amyotrophic lateral sclerosis: Dimethyl fumarate and H-151 downregulate inflammatory cytokines in the cGAS-STING pathway,” was published in the FASEB Journal.
ALS is a progressive neurodegenerative disease that affects motor neurons, the specialized nerve cells that control voluntary movement, in the brain and spinal cord. Motor neuron damage and death result in muscle weakness, breathing difficulties, and other symptoms that worsen over time.
While the exact causes of ALS remain largely unclear, they are thought to involve a combination of genetic and environmental factors. In sporadic ALS, the most common and non-inherited form of the disease, evidence suggests the involvement of inflammation and autoimmunity, or abnormal immune attacks against the body’s own healthy molecules.
The UCLA team, along with a colleague at Saint John’s Cancer Institute, in California, first set out to assess exactly what immune cells are involved in sporadic ALS and how they behave over the course of the disease.
By analyzing spinal cord samples from a 68-year-old man with sporadic ALS, the researchers showed that the spinal cord was invaded by cytotoxic T-cells, a type of immune cell that can kill microbes and certain cells.
These cells tested positive for interleukin (IL)-17A, a pro-inflammatory molecule, and granzyme B, an enzyme that can trigger nerve cell death and long-lasting inflammation.
Future investigation and eventually clinical trials need to determine whether the combination of H-151 with DMF would be synergistic against autoimmune inflammation in [sporadic ALS] patients.
Study analyzed immune cells from 8 men with sporadic ALS, 4 healthy people
Given that immune cells travel from the blood to tissues throughout the body, the researchers analyzed the gene activity profile of immune cells in blood samples from eight men with sporadic ALS and four healthy people (three women and one man).
In the early stages of disease, genes coding for the pro-inflammatory molecules IL-12A, IFN-gamma, and TNF-alpha, as well as granzymes, were more active in patients than in healthy controls.
Later on, at more advanced stages of disease, immune cells turned on genes coding for IL-17B, a signaling molecule involved in autoimmune reactions, as well as two chemokines called CXCL9 and CXCL10. Chemokines can attract immune cells, including cytotoxic T-cells, into the brain and spinal cord.
In turn, genes coding for the anti-inflammatory molecules IL-10 and TGF-beta became less active over the course of the disease.
The researchers then tested whether certain medications — DMF and H-151 — could tone down these inflammatory and autoimmune signals linked to sporadic ALS.
Sold as Tecfidera by Biogen and also available as generic versions, DMF is an oral small molecule approved for treating multiple sclerosis and psoriasis, two autoimmune conditions. It works by reducing inflammation and modulating immune system activity.
H-151, an experimental treatment, can decrease the production of pro-inflammatory molecules by lab-grown immune cells. It suppresses a signaling pathway called cGAS/STING, which is involved in immune cell activation.
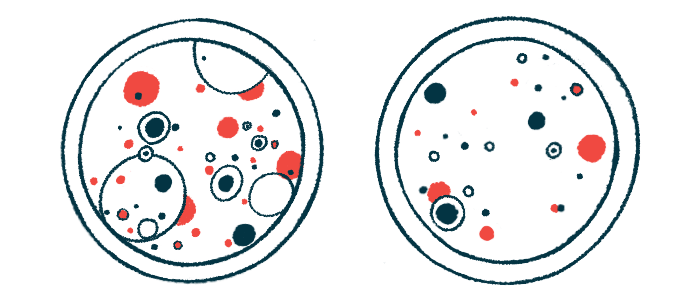
Lab-grown immune cells from two sporadic ALS patients, a 40-year-old man and a 65-year-old woman, were exposed to either DMF alone or in combination with EETs, or H-151.
EETs are a type of fatty molecule with anti-inflammatory effects that are derived from arachidonic acid, a polyunsaturated fatty acid (PUFA). PUFAs are generally considered good fats, being found in fatty fish, such as salmon and mackerel, seafood, nuts, and certain seeds.
Results showed that both DMF and H-151 reduced the activity of genes coding for granzymes and pro-inflammatory molecules, such as IL-6, IL-15, and IFN-gamma. The effect of DMF was even greater when combined with EETs.
Both medications suppressed inflammatory, autoimmune signaling in cells
These findings indicate that both medications suppressed “inflammatory and autoimmune signaling” in immune cells from sporadic ALS patients, the team wrote, supporting “their investigation in a clinical trial.”
The researchers noted that DMF has been previously tested in an ALS clinical trial, in combination with the standard treatment riluzole (sold as Rilutek, Exservan, and Tiglutik). Results showed that while the combination treatment was generally safe, it did not result in significant benefits in terms of ALS progression.
The current study’s results “suggest that DMF may be effective when combined with a diet rich in certain polyunsaturated fatty acids,” the team wrote.
“Future investigation and eventually clinical trials need to determine whether the combination of H-151 with DMF would be synergistic against autoimmune inflammation in [sporadic ALS] patients,” the researchers wrote. A synergy occurs when the combined effect of two medications is greater than the sum of their separate effects.