Nerve Cell Death Signaling May Hold Key to Treating ALS, Other Diseases, Study Finds
Written by |
A new process by which pro-death signaling is sent to nerve cells may hold the key for treating neurodegenerative diseases such as amyotrophic lateral sclerosis (ALS), which is characterized by the loss of motor nerve cells, according to researchers.
The study, “Retrograde degenerative signaling mediated by the p75 neurotrophin receptor requires p150glued deacetylation by axonal HDAC1,” was published in the journal Developmental Cell.
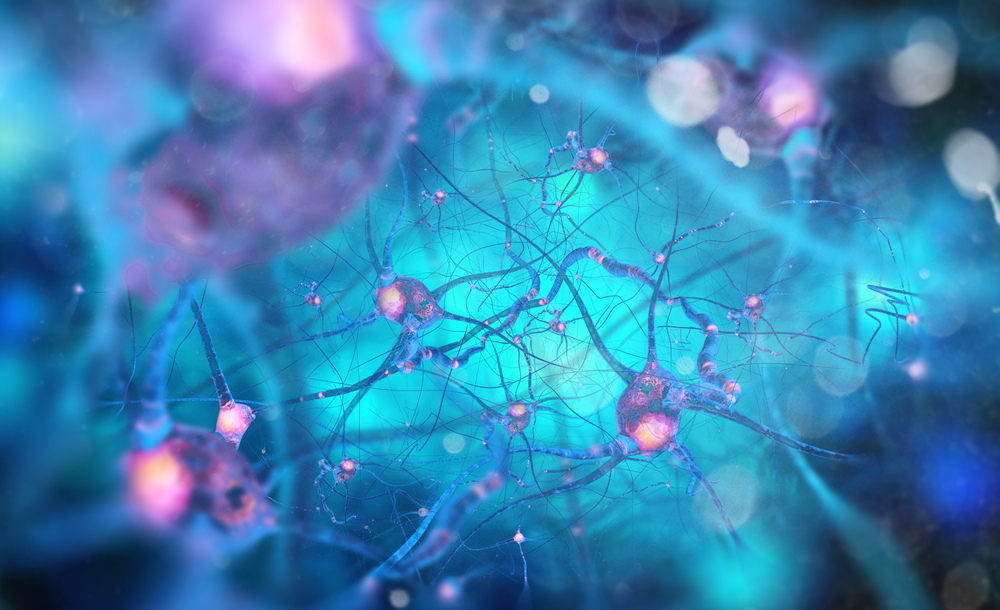
Neuronal apoptosis (programmed nerve cell death) is a necessary part of establishing proper neural circuitry. But when the regulation of apoptosis becomes abnormal and neurons start to die at a higher rate, neurodegenerative diseases can develop.
The balance between neuronal survival and death in the nervous system is governed by molecules called neurotrophic factors, such as neurotrophins. Neurotrophins exert their effects by binding to receptors on nerve cell endings.
Neurotrophins are produced by cells that neurons directly target and communicate with. So when a neuron relays a signal to a target cell, the target cell produces neurotrophins in response.
These neurotrophins can then go back and act on nerve cell endings to generate pro-survival signals that are conveyed from the nerve ending back to the body of the cell.
Due to the backwards nature of this phenomenon, it is called retrograde survival signaling.
Loss of neurotrophins leads to a reduction in pro-survival signals and an increase in pro-apoptotic (death) signaling. One of the ways researchers study this mechanism is through trophic deprivation therapy, or TFD.
Activation of p75 tyrosine kinase receptors (p75NTR) has also been implicated in apoptosis following TFD. To convey a retrograde apoptotic (pro-death) signal, a part of the p75NTR – known as the intracellular domain (ICD) – must be released.
The p75NTR ICD is taken from the nerve ending back to the body of the nerve cell, where it enacts the pro-apoptotic signal.
Researchers, therefore, hypothesized that the p75NTR ICD plays a key role in retrograde degenerative signaling and, as a result, cell death.
Retrograde signaling transport along the axon (a neuronal structure that carries a signal from the cell body to the target tissue and vice versa) is driven by the motor machinery of the cell which consists of a complex of proteins called dynein and dynactin.
“Formation of this complex and how it is regulated is still an active area of investigation,” researchers wrote.
Some studies have shown that proteins called histone deacetylases (HDACs) can play a role in axonal transport.
Therefore, researchers specifically investigated the role of HDAC1 in influencing p75NTR ICD-regulated retrograde degenerative signaling.
In fact, using a series of experiments, researchers show that p75NTR ICD and HDAC1 act as part of a retrograde pro-apoptotic signal that is generated in response to TFD or activation of p75NTR in neurons.
“We report an unconventional function of HDAC1 in retrograde transport of a degenerative signal and its constitutive presence in sympathetic axons,” the scientists wrote.
“There has been evidence of a retrograde degenerative signal, and now we’ve identified key components and a mechanism controlling their transport,” Bruce D. Carter, biochemistry professor and associate director of the Vanderbilt Brain Institute, said in a press release.
Importantly, these results have a clinical application. Mice with the G93A mutation in the SOD1 gene, which is associated with a form of ALS, were shown to have p75NTR ICD in association with dynein.
This suggests that the G93A mutation leads to pro-apoptotic signals in neurons and could explain neuronal cell death in patients with ALS.
“Hence, axonal transport of both pro-survival and pro-apoptotic signals needs to be considered in designing therapeutic strategies for neurodegenerative conditions,” the researchers wrote.