Plasma Creatinine Potential Biomarker of Functional Decline, Survival in ALS Patients, Study Indicates
Written by |
Levels of plasma creatinine — a metabolic product of healthy muscle — are significantly associated with the functional status of amyotrophic lateral sclerosis (ALS) patients, and can help predict their survival, results from a new study show.
The findings suggest that plasma creatinine may be an important biomarker to monitor ALS progression, particularly in patients without severe kidney disease, because rises in creatinine also may predict poor kidney function.
The study, “Plasma creatinine and oxidative stress biomarkers in amyotrophic lateral sclerosis,” was published in the journal Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration.
Biomarkers that help inform about disease progression are valuable tools to objectively measure the effectiveness of treatments, but they must be sensitive enough to demonstrate changes during the disease process.
In ALS, plasma creatinine has been proposed as a potential biomarker correlating with the progression of disease. Creatinine is a waste product of healthy muscle and a drop in its levels may indicate increased muscle wasting, which is a common symptom of ALS.
Because prior studies looking into this biomarker had certain limitations in their design, a team led by researchers at Columbia University Irving Medical Center in New York City set out to examine this biomarker in a well-controlled group of patients, using validated measures of disease progression.
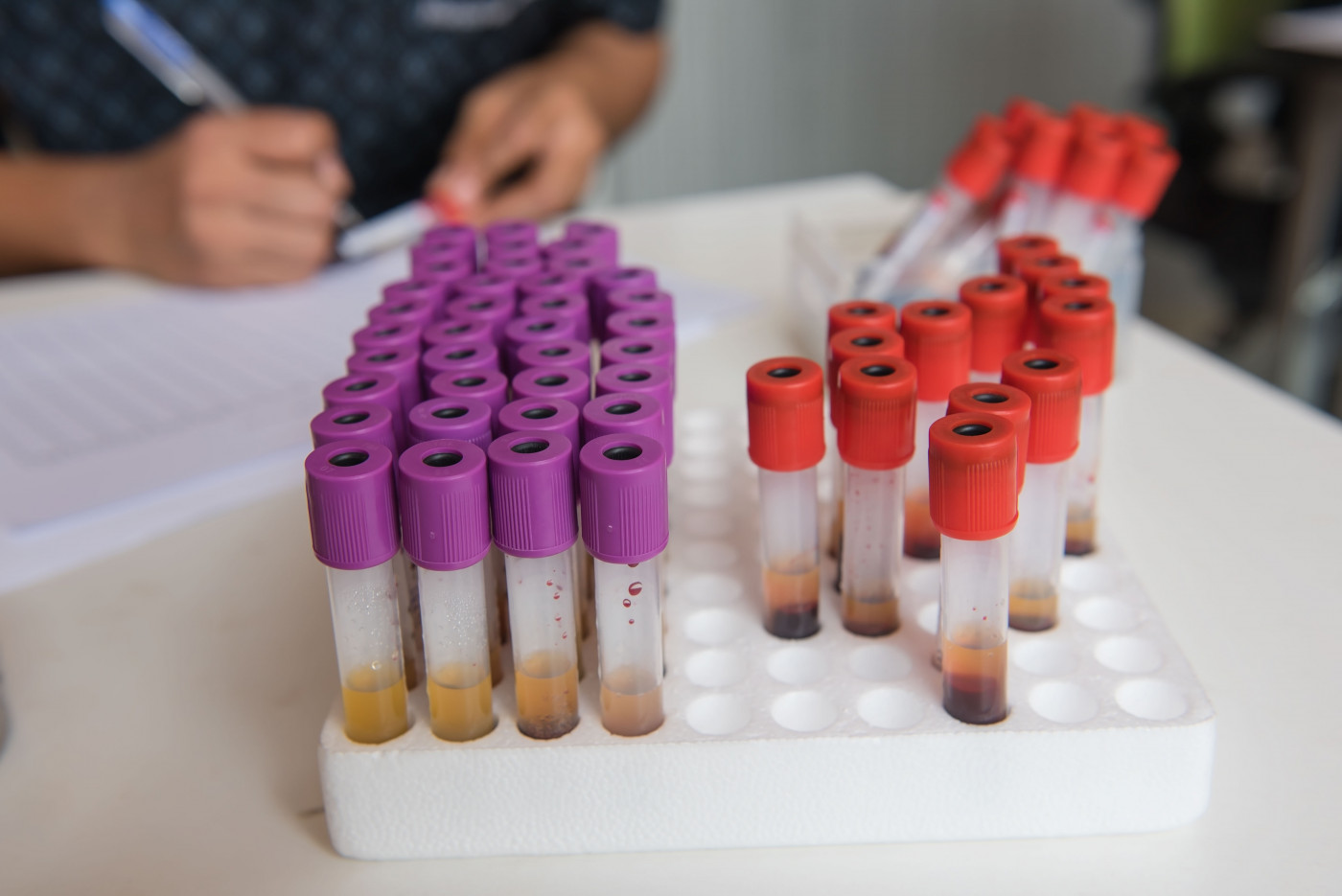
Participants were followed in a large prospective study — ALS COSMOS — originally designed to investigate the associations between oxidative stress and disease progression. It enrolled newly diagnosed patients, 61 years on average (age range 27 to 90), whose symptoms had started less than 18 months ago, and followed them until they died.
At study start (baseline) and at each follow-up visit, participants were assessed for measures of lung function (percent forced vital capacity, FVC), functional status (measured through the ALS functional rating scale-revised (ALSFRS-R) score), and provided blood and urine samples.
The researchers used data from these patients to examine if plasma creatinine at baseline correlated with measures of lung function and functional status at baseline, and in the last assessment before death (available for about 90% of patients).
They also examined other known biomarkers of ALS, such as the survival biomarkers urinary 8-oxodeoxy guanosine (8-oxodG) and 15- F2t-isoprostane (IsoP), as well as plasma uric acid (PUA), which predicts patient function and survival.
Results showed that levels of plasma creatinine at baseline significantly correlated with ALSFRS-R scores at baseline. After taking into account factors like age, sex, race, region of symptom onset, education, and months between symptom onset and enrollment, an analysis found that for each 0.1 mg/dL (milligrams per deciliter) increase in this biomarker, ALSFRS-R increased by 0.77 points.
At baseline, plasma creatinine also correlated positively with PUA and with lung function scores, and was negatively correlated with 8-oxodG levels.
A longitudinal analysis then demonstrated that plasma creatinine also correlated with ALSFRS-R scores at last visit and with longer survival time — for each 0.1 mg/dL increase in baseline creatinine, ALSFRS-R increased by 0.96 points and risk of death decreased by 12%.
Not surprisingly, higher functional status and lung function at baseline also were significantly associated with longer survival times. But baseline levels of PUA, urinary IsoP, and urinary 8-oxodG were not significant predictors of survival.
Notably, a combination of plasma creatinine, ALSFRS-R, and FVC — all measured at baseline — could explain about 56% of the variation in survival times, researchers found.
Finally, the Columbia team demonstrated that over the course of the study, ALSFRS-R declined by about 1.2 points per month, while plasma creatinine dropped by 0.02 mg/dL per month. These two measures correlated throughout the study, particularly in later stages of disease.
How each of these measures evolved over time in each patient also could predict survival, researchers found. Regardless of baseline levels, a patient whose creatinine levels dropped by 1 mg/dL throughout the study was 38% more likely to die, and for each one point decline in ALSFRS-R scores during the study, risk of death increased by 6%.
Overall, the findings “indicate that PCr [plasma creatinine] is strongly associated with ALS clinical progression and can also inform survival time,” the researchers wrote.
The team points to the lack of control patients as a limitation of their study, but says the use of a well-characterized ALS patient population, with extensive clinical information, is a clear strength.
While this biomarker is influenced by kidney function — making it nonspecific to ALS — the team suggests it may be used as a temporary, inexpensive biomarker in ALS patients without kidney problems, until novel biomarkers are clearly validated in ALS.