Restoring Levels of Membralin Protein May Extend Survival in ALS, Mouse Study Suggests
Written by |
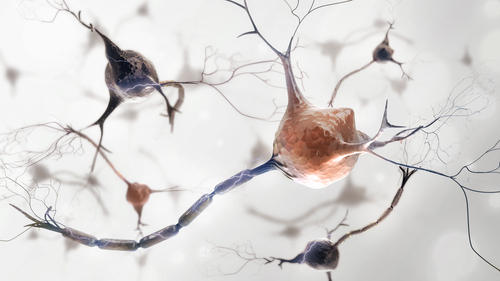
Low levels of membralin protein in the brain cells that support and protect neurons lead to the accumulation of the neurotransmitter glutamate to levels that induce the death of motor neurons in amyotrophic lateral sclerosis (ALS), a mouse study shows.
A gene therapy that rescued the levels of membralin prolonged the survival of mice with ALS, supporting the therapeutic potential of membralin-targeting therapies.
“This study provides an important new perspective into the mechanism(s) that may drive ALS, and a potential therapeutic direction, which are both critical first steps toward finding effective medicines,” John Ravits, MD, a study author and professor of clinical neurosciences at UC San Diego said in a press release.
The study, “Membralin deficiency dysregulates astrocytic glutamate homeostasis leading to ALS-like impairment” was published in The Journal of Clinical Investigation.
In ALS, there is a loss of neurons that control movement — the so-called motor neurons — in the brain and spinal cord, which comprise the central nervous system. When these neurons die, the control of voluntary muscles is gone, eventually affecting a person’s ability to swallow and breath. The cause behind ALS is still not clear, and there currently is no cure, only treatments that help manage the disease.
“ALS is a devastating condition in urgent need of new treatments. However, researchers are still grappling with the basics: what causes ALS and what causes it to progress,” Ravits said.
Now, researchers at Sanford Burnham Prebys in San Diego identified a protein called membralin that seems to play a key role in the development of ALS.
Researchers had previously shown that membralin is part of a protein disposal machinery called the endoplasmic reticulum-associated degradation system — a key protein quality control system. In fact, the protein was found to be important in preventing the accumulation of toxic aggregates, or clusters of proteins, that promote the development of Alzheimer’s disease.
To further understand the role of membralin in neurodegenerative diseases, the researchers now designed mice that lacked the protein altogether, in all the cells in the body. The scientists also designed mice that specifically lacked the protein in different brain cells, such as motor neurons and glial cells — cells that surround neurons and provide support. These glial cells include astrocytes, microglia and oligodendrocytes.
The investigators found that lack of membralin in astrocytes led to a loss of motor neurons in the spinal cord, and caused motor defects.
“We were surprised by the phenotypes of the membralin-lacking mice. They had clear muscle impairments that mirrored ALS symptoms in humans,” said Lu-Lin Jiang, postdoctoral researcher and the study’s first author.
“This finding was especially unexpected—and fortuitous—as previous genome-wide association studies (GWAS) had never identified the membralin gene as a potential culprit in ALS,” Jiang added.
Next, the team explored how membralin was involved in the development of ALS-like features. They found that lack of membralin caused an increased accumulation of the neurotransmitter glutamate outside astrocytes cells. Glutamate is a neurotransmitter that, when not properly cleared, is neurotoxic, meaning it kills neurons.
Moreover, the researchers saw that lack of membralin caused a decrease in the levels of the glutamate transporter, called excitatory amino acid transporter 2 (EAAT2). EEAT2 is the way that approximately 90% of glutamate is uptaken by cells of the central nervous system.
In animal models of ALS, and in spinal cord tissue from ALS patients — including both familial and sporadic types of the disease — the levels of EAAT2 and membralin were reduced, the researchers said.
Using a gene therapy in which membralin was delivered into the spinal cord of a mouse model of ALS, the researchers found that the mice lived almost two weeks longer than control mice, supporting the therapeutic potential for membralin-targeting therapies.
“These results indicated that membralin expression can reverse neurotoxic effects, extend lifespan,” the investigators said.
“Our study provided a mechanism for ALS pathogenesis where membralin limited glutamatergic neurotoxicity, suggesting that modulating membralin had potentials in ALS therapy,” the study concluded.