Blocking signaling pathways may reverse nerve cell changes in ALS
Stopping inflammation may help ease ALS symptoms, mouse study shows
Written by |
Blocking certain inflammatory signaling pathways may be one way to reverse nerve cell alterations that drive the symptoms of amyotrophic lateral sclerosis (ALS), according to preclinical research using a mouse model of the disease.
In the mice, an ALS-associated mutation in the FUS gene caused caused motor neurons — the nerve cells involved in motor control — to lose the branches and connections needed to function properly. It also disrupted cellular energy production and caused neuroinflammation, a complex inflammatory response typically seen within the brain or spinal cord.
A blockade of the inflammatory signaling pathway NF-kappa B was shown to reverse these cellular changes and improve motor and cognitive function in these animals.
In addition to further elucidating the role of FUS in driving ALS symptoms, the study indicates that “modulation of the [NF-kappa B] pathway … is an important therapeutic approach to attenuate disease,” the researchers wrote.
The study, “Neuronal dysfunction caused by FUSR521G promotes ALS-associated phenotypes that are attenuated by NF-κB inhibition,” was published in Acta Neuropathologica Communications.
Investigating the impact of FUS gene mutations on motor neurons
ALS is characterized by the degeneration of motor neurons, the specialized nerve cells involved in motor control. Mutations in FUS are thought to underlie the disease in about 5%-10% of people with familial ALS and less than 1% of those with sporadic ALS.
These mutations lead to the production of an abnormal version of the FUS protein that toxically accumulates in the wrong part of the cell. While the FUS protein is normally seen in the nucleus — the core of the cell where DNA is housed — ALS-associated FUS instead gathers outside the nucleus in the cytoplasm and disturbs cellular function.
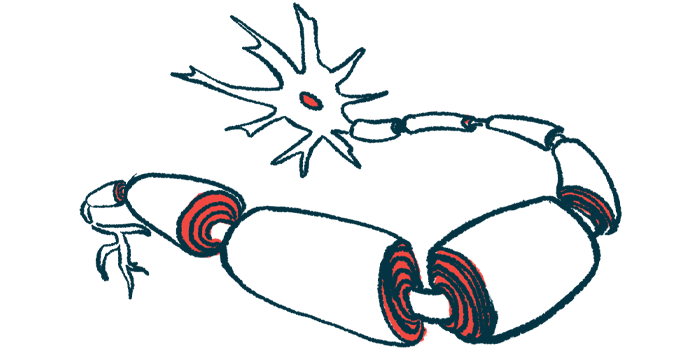
In mouse models, FUS mutations are associated with motor and cognitive deficits, activation of cells that promote inflammation, and structural changes to motor neurons that are also seen in the human condition. Specifically, motor neurons are found to lose dendrites, the branches they use to reach out to and communicate with other cells. The synapses, or connections, made with other cells via structures called dendritic spines also are lost.
Despite this knowledge, gaps still remain in scientists’ understanding of how FUS mutations lead to these neuronal changes and contribute to disease progression.
Now, a team of researchers from Laval University, in Canada, genetically engineered mice to house a human ALS-associated FUS mutation specifically in neurons, using them to further explore the effects of FUS.
At 1 month old, these mutant mice exhibited cognitive defects and reduced dendritic branching of upper motor neurons — the motor neurons that originate in the brain and travel to the spinal cord.
By 6 months of age, loss of dendritic branches and synapses had spread to affect the lower motor neurons, or those that travel from the spinal cord and innervate the muscles to coordinate movement. This was accompanied by progressive motor impairments.
A number of other cellular alterations also corresponded with the deteriorating cognitive and motor function of the mice. This included mis-localization of mutant FUS to the cytoplasm and signs of dysfunctional mitochondria, which are cells’ energy-producing organelles.
Moreover, activation of astrocytes and microglia, the nerve support cells (glia) that can drive neuroinflammation, was observed in the symptomatic mice.
Researchers use compound based on plant used in traditional Indian medicine
Activation of the NF-kappa B inflammatory signaling pathway — a series of molecular events that cells use to respond to signals of inflammation or infection — is thought to promote glial activation in ALS and other neurodegenerative diseases. That, in turn, has been linked to motor neuron damage and disease progression.
As such, the researchers aimed to investigate whether blocking inflammatory signaling might help restore more normal nerve cell connections and ease symptoms.
To that end, they treated the mice with the NF-kappa B inhibitor IMS-088, a synthetic compound based on the naturally occurring Ashwagandha plant.
That plant has been “used for thousands of years in traditional Indian medicine,” Chantelle F. Sephton, PhD, assistant professor at the University of Laval and the study’s senior author, said in a press release.
The treatment reversed many of the observed cellular deficits, leading to restored motor neuron dendrites and synapses, reduced glia activation, decreased FUS mis-localization, and increased mitochondrial function. This was accompanied by cognitive and motor improvements.
“Neurons regenerate without activated immune cells,” Sephton noted.
“The dendrites of motor neurons start to grow and make connections again, increasing the number of synapses between motor neurons and muscles,” Sephton said.
Lab studies of neurons from the mice further indicated that IMS-088 treatment promotes more normal mitochondrial function.
Altogether, the researchers believe the findings demonstrate the key role of neuroinflammation in ALS disease processes.
“Future studies will examine the mechanistic actions of inhibiting the [NF-kappa B] pathway on FUS function and the dynamic interplay between pro-inflammatory signals and mitochondrial function,” the team concluded.
The findings likely also have implications for other related diseases, including frontotemporal dementia (FTD), a neurodegenerative disease that has significant clinical and cellular overlap with ALS, as well as other inflammatory neurodegenerative conditions.