Interferon-gamma therapy may help delay familial ALS: Cell study
Interferon-gamma found to prevent oxidative stress in FUS-ALS motor neurons
Written by |
People with amyotrophic lateral sclerosis (ALS) due to mutations in the FUS gene may benefit from interferon-gamma treatment to delay disease onset and/or progression, an early preclinical study suggests.
Researchers found that an immune signaling protein called interferon (INF)-gamma protected patient-derived motor neurons from oxidative stress.
INF-gamma also restored the activity of genes that normally respond to oxidative stress, a type of cellular damage implicated in the disease, and improved overall protein production within motor neurons, which is compromised in FUS-related ALS.
The cell-based study, “IFNγ protects motor neurons from oxidative stress via enhanced global protein synthesis in FUS-associated amyotrophic lateral sclerosis,” was published in the journal Brain Pathology.
FUS gene mutations account for 5% of familial ALS, 1% of sporadic cases
Mutations in the FUS gene, which encodes a protein of the same name, cause about 5% of familial ALS and about 1% of sporadic ALS cases. FUS mutations have been associated with the most aggressive forms of ALS, including a type that occurs in adolescents and young adults.
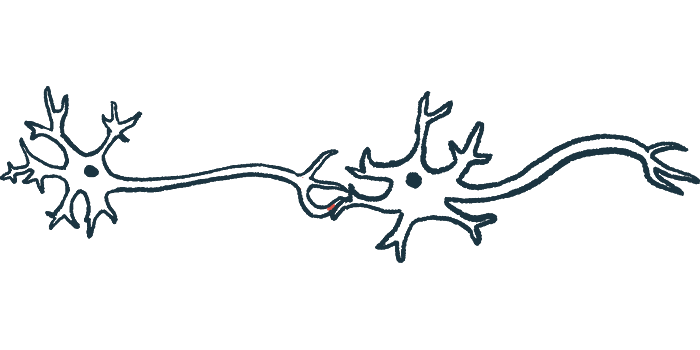
FUS protein is typically found in the cell nucleus and plays various roles in protein production. However, exactly how these mutations cause the death of motor neurons, the nerve cells that control voluntary movements, which lead to ALS symptoms, is still unclear.
To reveal biological defects caused by FUS mutations, scientists in the Netherlands and Brazil generated motor neurons derived from ALS patients who carried FUS-R521H, a prominent ALS mutation. Control cells were derived from family members who did not have ALS.
Results showed that cell viability, or the proportion of healthy cells, was similar between the control and FUS-ALS motor neurons. However, when exposed to sodium arsenite, a well-known inducer of oxidative stress, mutant cells were significantly less viable than controls.
FUS-ALS motor neurons more sensitive to oxidative stress
FUS-ALS motor neurons were “more sensitive to oxidative stress,” the scientists noted.
Gene activity experiments revealed oxidative stress sensitivity of motor neurons might be explained by changes in genes related to the immune system and two major signaling pathways: TGF-beta and mTORC, both essential for proper cell function.
Consistent with TGF-beta’s role in the production of immune signaling proteins called cytokines, FUS-ALS motor neurons, when exposed to sodium arsenite, produced more interleukin-8 and CCL2 cytokines and less INF-gamma and interleukin-15. In control cells, INF-gamma increased with sodium arsenite exposure, something that FUS-ALS cells failed to do, the team noted.
Because mTORC and FUS both have known roles in protein production, the researchers also measured the rates of protein synthesis. Overall, FUS-ALS motor neurons had lower rates than control cells, but no differences were noticeable in gene activity, which was “in agreement with findings of others.”
Significantly decreased protein production rates were also found in healthy cells engineered to overproduce FUS-R521H. This suggested that the FUS mutation resulted in an overly-active FUS protein in ALS motor neurons, rather than in reduced levels of FUS.
Our findings suggest that early-diagnosed [FUS-ALS] patients might benefit from [INF-gamma] treatment to slow down disease progression.
ALS motor neurons more susceptible to cell death
ALS motor neurons are “more susceptible to apoptosis [cell death] due to decreased protein synthesis rates caused by an R521H gain-of-function [overactive] mutation in the FUS gene,” the researchers wrote.
In healthy cells, FUS is known to move between the cell nucleus and the cytoplasm (the gelatinous liquid that fills the inside of a cell). In ALS, however, FUS is mainly found in the cytoplasm of motor neurons, which ultimately leads to FUS clumping.
Consistently, in FUS-ALS motor neurons, FUS levels were reduced in the nucleus and increased in the cytoplasm. Protein interaction studies showed that, when in the cytoplasm, FUS-R521H binds to various proteins that initiate protein synthesis.
The abnormal localization of FUS-R521H was also found in cells harboring mutations that cause other forms of ALS.
“These findings suggest that aberrant cytoplasmic localization of FUS is common among ALS subtypes,” the scientists wrote, and “leads to promiscuous binding of FUS to cytoplasmic proteins with a role in [protein production].”
INF-gamma treatment decreased cell death to control levels
Finally, treatment with INF-gamma, which was reduced in FUS-ALS motor neurons, increased mutant cell viability after sodium arsenite exposure and decreased cell death to control levels. INF-gamma treatment also rescued the impaired gene activity seen in response to oxidative stress.
Although the treatment did not affect protein synthesis rates in control cells, it significantly increased them in FUS-ALS motor neurons, with or without sodium arsenite exposure.
INF-gamma treatment also increased FUS levels in the nucleus, almost to those in control cells. In agreement, suppressing levels of FUS improved protein synthesis rates in FUS-R521H cells and reduced cell death, similar to INF-gamma.
“While further work is required to understand how [INF-gamma] restores FUS localization and impaired translation rates, our findings suggest that early-diagnosed [FUS-ALS] patients might benefit from [INF-gamma] treatment to slow down disease progression,” the researchers concluded.