Living with ALS
After a diagnosis of amyotrophic lateral sclerosis (ALS), a progressive neurodegenerative, muscle-wasting condition that doesn’t have a cure, your focus should be on what you can do to help maintain your quality of life.
ALS, also known as Lou Gehrig’s disease, is commonly classified into two main types — familial and sporadic. Symptoms generally appear earlier in the familial type, which means there is a family history of ALS.
About 90% of cases are categorized as sporadic ALS. This means the disease doesn’t follow a clear pattern, meaning individuals have no known family history of the disease.
One of the early signs of ALS is muscle weakness. At first, the weakness may be barely noticeable and affects just one part of the body. But as it progresses, the muscle weakness tends to become more severe and spread to other areas.
How does ALS affect daily living?
ALS affects the body in a number of challenging ways, but especially affects mobility, breathing, communication, and mental health. These symptoms will worsen over time.
To help navigate these and other ALS-related changes, planning and coping strategies are required for daily living, as are the use of adaptive devices and technologies, therapeutic treatments, exercise and diet modifications, mental health care, and making your living space more accessible. The overall goal is to manage symptoms to maintain health and independence for as long as possible.
Muscle weakness
About 70% of people living with ALS have limb onset ALS. This type of the disease causes muscle weakness, particularly of the arms and legs, and can affect mobility and the ability to coordinate movements.
Usually, the first muscles affected are the distal muscles, those further from the torso, such as those in the hands, feet, calves, and forearms. When it affects the upper limbs, it can make tasks like writing difficult, while weakness in the lower limbs often makes walking difficult.
Bulbar weakness
Bulbar-onset disease, seen in about 25% to 30% of ALS patients, first affects the muscles around the face and throat. These muscles in the head and neck are called the bulbar muscles. Difficulty swallowing and/or speaking are the most common early symptoms in bulbar-onset ALS.
Difficulty breathing
People living with ALS often experience chronic respiratory failure due to weakness in the muscles of the chest and diaphragm. Weakness in the respiratory system can lead to problems with breathing and frequent lung infections. Eventually, a ventilator to support breathing may be required.
Cognitive decline
Cognitive (brain-related) and behavioral changes have been observed in people living with ALS, with approximately half of patients having one or both ALS-related changes at some point.
Between 10 and 15% of people will experience frontotemporal decline, a form of dementia.
ALS treatment options
While there’s no cure for ALS, approved treatments can help manage the condition. Some help with symptoms while others are aimed at the underlying cause of the disease. There are also a number of experimental treatments for ALS.
Supportive treatments can include speech therapy, occupational therapy, and physiotherapy.
People living with ALS often deal with chronic respiratory failure, which will worsen over time. Supportive options may eventually be required, such as a tracheostomy, where a hole is opened in a person’s windpipe to provide an alternative way to breathe, chronic ventilatory support, and noninvasive positive pressure ventilation.
It is recommended that you discuss with your healthcare team the best way to manage these symptoms soon after diagnosis and that it becomes part of an ongoing conversation.
Difficulty swallowing can cause weight loss. Losing weight, especially in the first few years, may worsen the prognosis of ALS. A change in diet may be needed to include calorie-dense foods and supplemental nutritional beverages.
Depending on the circumstances, your healthcare team may suggest placing a gastronomy, or feeding tube, to ensure food is delivered to the stomach.
Some people living with ALS may experience the pseudobulbar affect (PBA, or emotional lability), which causes laughing or crying that doesn’t reflect your actual mood or feelings. Nuedexta may be prescribed for treating PBA.
Treatment may also include cognitive and behavioral therapy to address behavioral changes, depression, and dementia.
Creating a daily routine
Living with ALS means making changes to how you take care of both the small and large tasks of your daily routine.
This includes grooming, getting dressed, sleeping and organizing medication, as well as more complicated activities, such as traveling and driving a motor vehicle.
There are guides that give advice for tackling the challenges of everyday living with ALS, including:
- Daily Activities Made Easier for People Living With Amyotrophic Lateral Sclerosis (ALS)
- Everyday Life with ALS
- ALS & Activities of Daily Living
- ALS Guide.
Dagmar Munn was diagnosed with ALS in 2010 when she was 59. After she made peace with the abrupt change to her life, she learned to focus on the present.
“Worries about our future can be dialed down by taking time to list solutions,” she wrote in “Taking the time to mentally exhale while living with ALS” for ALS News Today.
The former yoga and dance teacher and fiber artist wrote about the four strategies she incorporates into her daily routine to help manage her medications, mindfulness, motion, and mood. They are:
- “follow your doctor’s advice and take all prescribed medications”
- “practicing mindfulness has helped me feel that I am in control, have more awareness, and am moving safely”
- “moderate exercise can improve life span and ease ALS symptoms”
- “when I notice that I’m having trouble coping with change, I ask myself what has changed, what I need to do or who can help me.”
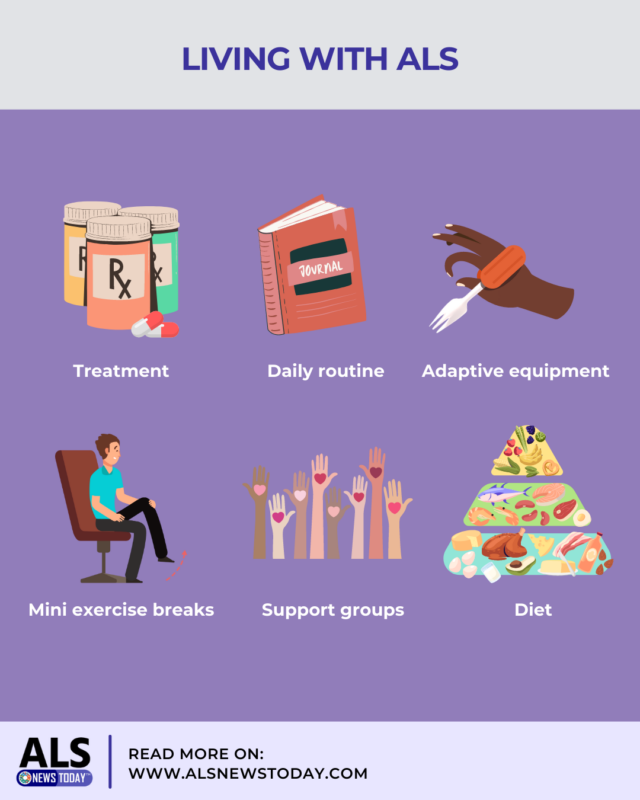
Adaptive equipment
Adaptive devices for living with ALS include aids for eating and drinking, getting dressed, bathroom activities such as bathing, toileting, oral care and grooming, voice-activated house controls, and devices to aid in recreation and mobility.
Adaptive devices include:
- a cane, rollator, wheelchair, grab bars, and orthotic braces to aid mobility
- built-up utensils, a universal cuff to aid in holding utensils, arm supports, and specialized drinking cups to aid eating and drinking
- wearing adaptive clothing with features like elastic waists, velcro or magnetic closures, shoes without laces, and using tools such as a dressing stick, buttoner, and zipper pull to make dressing easier
- picture boards, computers with text-to-speech, and eye-gaze devices to make communicating easier
- smart home electronics with voice-activated controls or input from a tablet or smartphone to help with tasks like lighting levels, temperature control, and answering the door.
Munn wrote about her changing feelings toward a rollator after her lower limbs became weak and unreliable, and her neurologist suggested she try using one.
At first, she resisted. Eventually, she learned to appreciate its usefulness and the safety it offered. Now, she can’t imagine life without her rollator.
“Looking back,” she wrote, “I realize that the evolution of my mindset from initially disliking rollators to wanting to improve them, to now liking mine just the way it is, has come a long way.”
Physical therapy and exercise
Exercising under the guidance of a physical therapist is still considered controversial in managing ALS.
The general goal of exercise is to build muscle through resistance training and pulmonary and respiratory capacity through aerobic exercises.
According to one 2021 study, which reported a meta-analysis of the role of prescribed exercise in managing ALS, exercise can be beneficial for people living with ALS, but more comprehensive research is needed.
The study said exercises for people living with ALS should:
- minimize the risk of falls
- avoid high-resistance exercises to prevent fatigue.
Munn wrote about the role of exercise in her life, noting “long bouts of uninterrupted sitting can have negative physical and emotional consequences.”
She created an exercise plan that lets her safely do mini-sessions of exercise throughout the day, including for her legs, arms, and glutes.
“I do a few repetitions instead of a long, tiring sequence of movements each time,” Munn says. “It’s enough to fire up my muscles, but not tire them out.”
Diet
Difficulty swallowing, or dysphagia, can cause a nutritional deficit for people living with ALS and lead to excessive weight loss, fatigue, weakness, and, in some cases, loss of appetite and faster disease progression.
It may be helpful to seek professional help about recommended ALS diets and nutritional information, as well as adaptive devices for eating and drinking. Surgery to place a feeding tube may eventually be needed.
Following a balanced diet of grains, vegetables, fruit, dairy, and proteins, and increasing caloric intake of heart-healthy fats and oils, such as olive oil is generally recommended.
Registered dietitian Alanna Kessler wrote about how to optimize the ALS diet and the use of supplements for ALS News Today. Among her dietary suggestions are:
- increasing dietary fiber as it lowers inflammation and promotes gut health
- vitamin B12 supplementation, a water-soluble vitamin that plays an essential role in the homeostasis (proper functioning environment) of the nervous system
- carnitine, an essential antioxidant that protects against oxidative stress and damage, which can be found in red meats as well as chicken, milk, beans, avocado, milk, and fish.
Emotional support
Dealing with ALS-related changes and symptoms can be as difficult emotionally as it is physically.
Since a person’s emotional well-being can have a significant effect on general health and quality of life, seeking out professional help and joining in-person and online ALS support groups can be an emotional lifeline.
Support groups bring together people living with ALS into a peer-led community for sharing experiences, advice, and strategies for managing emotions.
The International Alliance of MND/ALS Association offers a list of country-specific organizations around the globe, many of which offer in-person and online support.
You can also join Bionews’ ALS News Today Forums.
Finding something you enjoy is also important. The activities are up to you, but they can be as varied as listening to audiobooks, writing in a journal, or going fishing with assistance.
In “How Journaling Helped Me Adjust to Living With ALS,” Munn writes about how keeping a journal helped her track her day-to-day symptoms to discuss with her healthcare team and also provided her with some emotional self-reflection.
“Writing in my little notebook at the end of each day kept me focused on my goals and on track with daily exercises,” says Munn. “It was a welcome therapeutic method to sort through my negative feelings about having ALS.”
Life expectancy and palliative care
Life expectancy varies greatly for people living with ALS. A number of factors are associated with shorter ALS survival, including the bulbar onset form of the disease, a delay in diagnosis, frontotemporal dementia, older age at onset, and pronounced weight loss. Genetic factors can also affect survival.
The American Academy of Neurology, the European Network for the Cure of ALS, and ALS Canada have guidelines for palliative care for people with ALS.
Palliative care is multidisciplinary treatment for a terminal illness, such as ALS, and hospice may be considered. Treatment includes controlling symptoms, including for pain and difficulty breathing, or dyspnea.
Palliative care may be discussed soon after diagnosis. You should also have an advance care plan written by the person living with ALS.
ALS News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- New collaboration targets protein buildup linked to brain diseases
- New funding backs commercial readiness efforts for ALS therapy
- US lawmakers reintroduce bill to improve access to treatment for ALS
- An emotional dance performance mirrored my life with ALS
- Expanded access program for ALS drug MN-166 at 50% enrollment
 Fact-checked by
Fact-checked by