Compound Works to Ease Brain Inflammation Driven by Glial Cells
A molecule that blocks the regulatory RNA protein HuR, called SRI-42127, strongly reduces brain inflammation driven by activated glial cells, key players in neurodegenerative diseases like amyotrophic lateral sclerosis, a preclinical study reported.
This inhibitor may be of promise in treating ALS and other diseases driven by inflammation in the brain.
“Our findings underscore HuR’s critical role in promoting glial activation and the potential for SRI-42127 and other HuR inhibitors to treat neurological diseases driven by this activation,” Peter King, MD, and Burt Nabors, MD, professors of neurology at the University of Alabama at Birmingham, said in a press release.
The study, “SRI-42127, a novel small molecule inhibitor of the RNA regulator HuR, potently attenuates glial activation in a model of lipopolysaccharide-induced neuroinflammation,” was published in Glia.
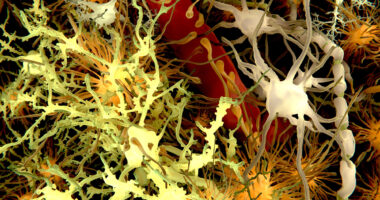
Microglia and astroglia (glial cells) are immune cells that work to protect the brain from infections and trauma. Upon activation, they produce a range of inflammatory proteins that help to eliminate invading agents.
However, glial cells can produce excessive quantities of inflammatory proteins, some of which attract other immune cells, including neutrophils and monocytes, which in turn produce more inflammatory proteins and cause severe damage.
HuR is an RNA-binding protein that regulates the amount of inflammatory proteins produced by activated glial cells. RNA is most typically the intermediate molecule that originates from genes to produce a protein, but some RNA molecules also have regulatory functions.
HuR normally resides in the cell nucleus, but moves into the cytoplasm when cells are activated, boosting the production of inflammatory proteins.
Of note, HuR can only leave the nucleus when two HuR molecules combine to form a dimer, a compound consisting of two similarly structured single molecules. The inhibitor identified by this study’s scientists, SRI-42127, works by blocking HuR dimerization, preventing it from moving into the cytoplasm and activating the production of inflammatory proteins.
Because dimerization is crucial for HuR’s inflammatory effects, King and Nabor, working with university colleagues, investigated whether SRI-42127 could lessen the inflammatory response of glial cells.
The researchers used lipopolysaccharide (LPS), one of the main cell surface components of bacteria, to activate glial cells initially in lab dishes (in culture) and later in animals. As expected, LPS stimulation caused HuR to move from the nucleus to the cytoplasm in most of lab-grown glial cells, and significantly increased their production of pro-inflammatory proteins, such as interleukin-6 (IL-6), iNOS, and CXCL1.
Treatment with SRI-42127, however, prevented HuR’s migration, and significantly lowered the levels of the pro-inflammatory molecules, without impacting the production of anti-inflammatory proteins.
Similar experiments in mouse models confirmed these findings: SI-42127 was able to significantly lower the amounts of inflammatory proteins produced by activated glial cells, with minimal effect on anti-inflammatory proteins.
The scientists also found that SI-41227 could lower the number of neutrophils and monocytes migrating into the mice’s brains after LPS stimulation.
“We have used lipopolysaccharide-induced glial activation to show that SRI-42127 blocks HuR [movement from the nucleus to the cytoplasm] in glial cells, attenuates production of key pro-inflammatory [molecules], dampens glial activation and the infiltration of neutrophils and monocytes into the central nervous system (CNS),” the researchers wrote
While “SRI-42127 may represent a promising new approach for treatment of neurological diseases driven by neuroinflammation,” more research is warranted to determine at which phase of the neurodegeneration process it will have the greatest benefits.
“Therapeutic targeting of glia in CNS [central nervous system] disease is a balancing act since these cells also exert neuroprotective and neuroplastic effects depending on the phase of recovery from CNS injury or stage of neurodegenerative disease,” they wrote.